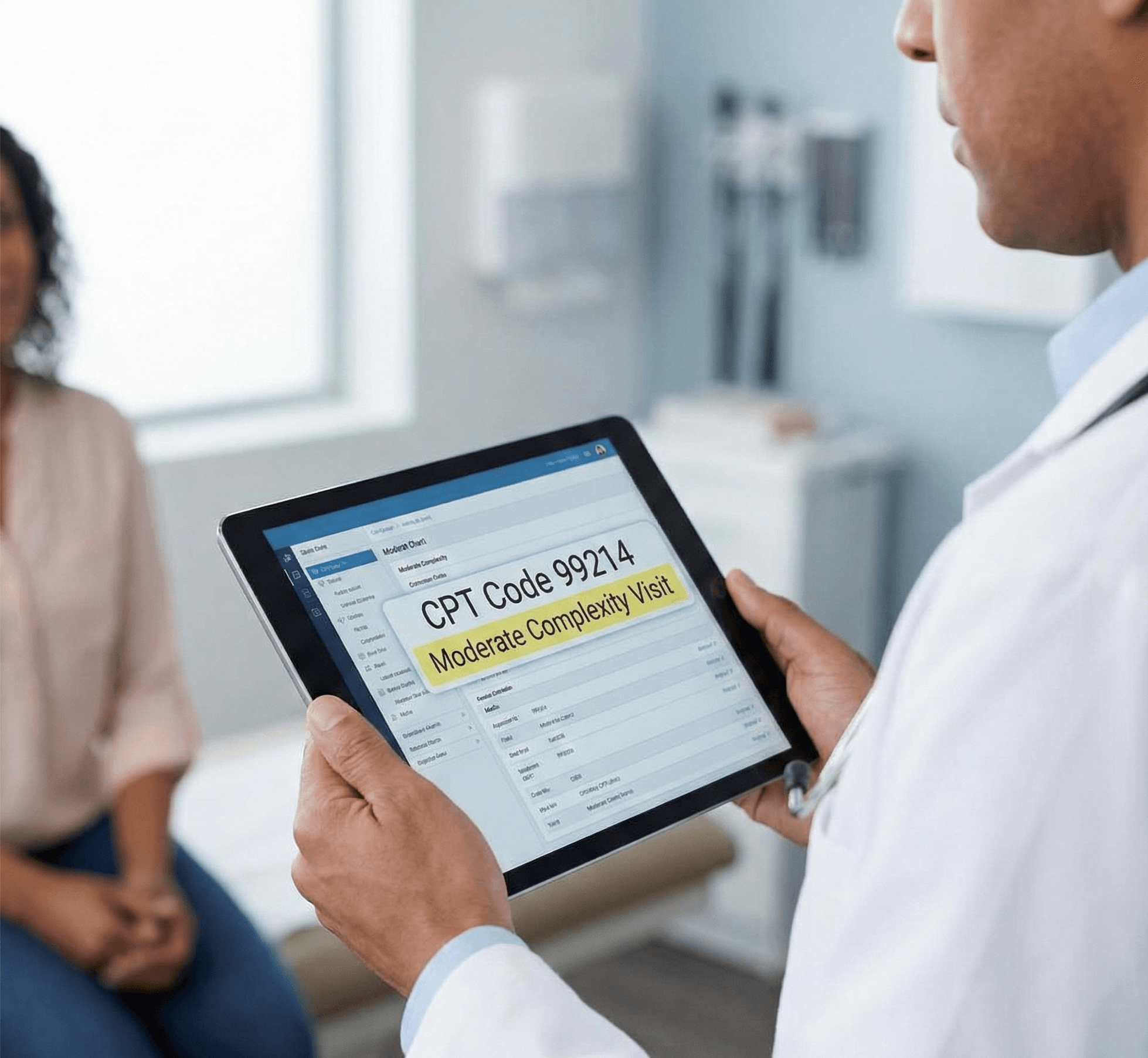
Understanding CPT Code 99214: Your Most Frequently Used E/M Code
CPT 99214 represents a moderate-complexity evaluation and management (E/M) service for established patients in office or outpatient settings. For mental health providers, particularly psychiatrists, this code often becomes the backbone of their billing practice, striking the perfect balance between appropriate reimbursement and documentation requirements.
Unlike the high-complexity 99215, CPT 99214 fits a large portion of routine psychiatric follow-up visits where patients require ongoing medication management, therapeutic interventions, and care coordination. This comprehensive guide will help you understand when to use 99214, how to document appropriately, and maximize your practice's efficiency while maintaining compliance.
Current Billing Requirements for CPT Code 99214
Following the 2021 E/M guideline changes, billing for 99214 has become more straightforward. You can qualify for this code through either of two pathways:
Option 1: Time-Based Billing
- Minimum 30 minutes of total provider time on the date of encounter
- Includes all provider activities on encounter date
Option 2: Medical Decision-Making (MDM)
- Moderate complexity medical decision-making
- Requires meeting 2 of 3 MDM elements at the moderate level
The elimination of history and physical exam as required elements means providers can focus on clinically relevant documentation rather than checking boxes.
Moderate-Complexity Medical Decision-Making Explained
Moderate-complexity MDM requires meeting at least two of these three elements:
1. Number and Complexity of Problems Addressed
Moderate level requires one or more of the following:
- Two or more stable chronic illnesses
- One or more chronic illnesses with exacerbation or progression or side effects of treatment
- One undiagnosed new problem with uncertain prognosis
- One acute illness with systemic symptoms
- One acute complicated injury
Mental health example: A patient with stable bipolar disorder and generalized anxiety disorder requiring medication adjustment due to breakthrough anxiety symptoms.
2. Amount and/or Complexity of Data Reviewed
Moderate level requires meeting one of these categories:
- Review of prior external notes from unique source + review of the results of each unique test + ordering of each unique test + assessment requiring independent historians (three out of four required to meet this level)
- Independent interpretation of a test performed by another physician or qualified health professional
- Discussion of management or test interpretation with external physician/other qualified health professional/appropriate source
Mental health example: A direct phone call or verbal exchange with the patient's Primary Care Physician or Cardiologist to discuss the safety of adding a new medication that may affect their QTc interval.
3. Risk of Complications and/or Morbidity
Moderate level includes:
- Prescription drug management
- Decision regarding minor surgery with identified risk factors
- Decision regarding elective major surgery without identified risk factors
- Diagnosis or treatment significantly limited by social determinants of health
Mental health example: Adjusting antidepressant dosage, adding mood stabilizer, or managing multiple psychiatric medications with attention to drug interactions.
Common Clinical Scenarios for 99214 in Mental Health
Typical 99214 Encounters Include:
Medication Management Visits:
- Routine follow-up for stable depression and anxiety
- Adjusting SSRI or SNRI dosages
- Managing ADHD medications with monitoring
Complex Follow-ups:
- Partial response to treatment requiring modification
- Managing side effects while maintaining therapeutic benefit
- Addressing medication non-compliance issues
Initial Stabilization:
- Second or third visit after starting new medication
- Early treatment response assessment
- Titration visits for mood stabilizers or antipsychotics

Time-Based Billing: Maximizing Your 30-39 Minutes
When billing based on time, document all qualifying activities:
Pre-service work:
- Chart review and preparation (5-10 minutes)
- Reviewing prior visit notes and treatment response
- Checking prescription monitoring database
Face-to-face time:
- Mental status examination
- Symptom assessment and rating scales
- Medication education and counseling
- Treatment planning discussion
Post-service work:
- Medical record documentation
- Prescription writing and e-prescribing
- Brief care coordination
- Responding to pharmacy clarifications
Real-world example: Total time: 35 minutes
- 5 minutes: Pre-visit chart review and PDMP check
- 25 minutes: Face-to-face psychiatric evaluation and medication management
- 5 minutes: Documentation and prescription management
Appropriate ICD-10 Codes for 99214 Encounters
It is important to note that ICD codes do not determine billing. However, common mental health diagnoses that typically support 99214 complexity include:
- F32.1 - Major depressive disorder, single episode, moderate
- F33.1 - Major depressive disorder, recurrent, moderate
- F41.1 - Generalized anxiety disorder
- F31.9 - Bipolar disorder, unspecified
- F90.2 - Attention-deficit hyperactivity disorder, combined type
- F43.10 - Post-traumatic stress disorder, unspecified
- F41.0 - Panic disorder without agoraphobia
- F42.9 - Obsessive-compulsive disorder, unspecified
Using specific, accurate ICD-10 codes strengthens medical necessity and supports your billing.
2025 Medicare Reimbursement and Payment Considerations
Current Medicare reimbursement for 99214 typically ranges around ~$125/visit depending on geographic adjustments (based on CMS Physician Fee Schedule). This represents approximately 70-75% of the 99215 reimbursement rate, making it a sustainable code for routine psychiatric care.
Commercial insurance rates often exceed Medicare by 20-40%. Always verify specific rates with individual payers, as contracts vary significantly.
Psychotherapy Add-On Codes
When providing psychotherapy with medication management, add the appropriate code:
- +90833: 16-37 minutes of psychotherapy with E/M
- +90836: 38-52 minutes of psychotherapy with E/M
These add-on codes increase total reimbursement while accurately reflecting services provided. These codes can only be added when 99214 is billed using E/M guidelines, not time-based billing.
99213 vs 99214 vs 99215: Making the Right Choice
Use 99213 (low complexity) when:
- Single stable chronic condition
- Minimal medication adjustment
- 20-29 minutes total time
- Routine refill with stable symptoms
Use 99214 (moderate complexity) when:
- Multiple stable conditions or one with exacerbation
- Prescription drug management
- 30+ minutes total time
- Moderate risk requiring monitoring
Use 99215 (high complexity) when:
- Severe exacerbation or multiple unstable conditions
- High-risk medication changes
- 40+ minutes total time
- Significant safety concerns or hospitalization consideration
Documentation Best Practices for 99214
Essential Documentation Elements:
Chief Complaint: Brief, specific reason for visit
History of Present Illness: Document relevant interval history including:
- Treatment response since last visit
- Medication compliance and side effects
- Functional status changes
- Relevant psychosocial factors
Assessment and Plan: Clearly articulate:
- Current stability of each diagnosis
- Medication changes and rationale
- Monitoring parameters
- Follow-up interval and reasoning
Sample Documentation:
"35-year-old with MDD and GAD, moderate severity. Partial response to sertraline 100mg daily - depression improved (PHQ-9 decreased from 15 to 10) but residual anxiety persists. No side effects reported. Increasing sertraline to 150mg daily. Discussed expected timeline for improvement and potential side effects. Continue weekly therapy. Follow-up in 4 weeks to assess response. Total time: 32 minutes."
Compliance Tips and Common Pitfalls
Avoid These Common Errors:
- Undercoding stable complex patients - Multiple stable conditions can support 99214
- Defaulting to 99213 for all follow-ups without assessing complexity
- Incomplete time documentation - Specify activities and total time
- Generic documentation that doesn't reflect individual patient needs
- Missing the moderate complexity threshold by not documenting data review
Optimize Your Practice:
- Use structured templates that prompt complete documentation
- Implement rating scales (PHQ-9, GAD-7) to demonstrate data review
- Document care coordination efforts, even brief communications
- Consider practice management software with built-in coding guidance
- Regular coding audits to ensure consistency
Leveraging Technology for Accurate 99214 Coding
Modern AI-powered documentation assistants can streamline 99214 billing by:
- Automatically calculating encounter time
- Analyzing documentation for MDM complexity
- Suggesting appropriate CPT codes based on visit content
- Ensuring documentation completeness for audit protection
- Generating compliant notes while maintaining clinical relevance
Conclusion
CPT code 99214 serves as the workhorse of mental health E/M billing, appropriately capturing the complexity of most psychiatric follow-up visits. By understanding the moderate complexity requirements and implementing strong documentation practices, providers can ensure accurate reimbursement while focusing on patient care.
The flexibility to bill based on either MDM or time allows providers to choose the most appropriate method for each encounter. With proper documentation and attention to coding guidelines, 99214 can effectively represent the valuable services mental health providers deliver daily.
Remember that coding guidelines and payer policies evolve. Stay informed through regular updates from the AMA, CMS, and your professional associations to maintain compliance and optimize reimbursement. Level up your medical writing – try Medwriter.ai now and simplify your workflow.
FAQs
What is CPT code 99214?
CPT 99214 is a medical billing code used to report an office or other outpatient visit for the evaluation and management of an established patient.
According to current coding guidelines, a 99214 visit requires a medically appropriate history and/or examination and must meet one of the following two criteria:
- Medical Decision Making (MDM): The level of decision making must be Moderate. This is often, but not always, characterized by certain prescription drug management, the diagnosis of a new problem with uncertain prognosis, or management of two or more stable chronic illnesses.
- Total Time: The total time spent on the date of the encounter is 30–39 minutes. This includes face-to-face time and non-face-to-face time (charting, ordering tests) on the same day.
Note: You do not need to meet both criteria; you may select the code based on whichever method (MDM or Time) is most advantageous for that specific encounter.
What is the difference between 99213 and 99214?
The difference is the level of severity and time. 99213 represents Low Complexity (20–29 minutes) and is often used for stable chronic conditions or minor acute injuries. 99214 represents Moderate Complexity (30–39 minutes) and is often appropriate when a patient’s chronic condition is worsening, a new problem arises, or prescription medication is managed.
To see a full breakdown of the differences, reference this chart.
How much can you bill for 99214?
There is no legal cap on what a practice can charge (your billed amount).
How much does 99214 pay? / What is the reimbursement for CPT code 99214?
Reimbursement depends on the payer and your specific geographic location. As of 2024-2025, the Medicare national average is approximately $126–$129. Private insurance carriers can pay higher than Medicare.